CHM members are free to choose their own healthcare providers, take advantage of our preferred CHM providers (who give unique discounts to CHM members), or use a provider we’ve helped you select for certain medical events (maternity or non-emergency surgical procedures). Our CHM Care Solutions offer specialized care components to help you navigate your healthcare journey, often leading to savings, superior treatment and peace of mind. For example, you can also use HealthTap providers through our Virtual Care Solution for your primary or urgent care needs.
Whether you choose to use a provider CHM recommends or another provider, we can give you the tools to effectively communicate with your provider about your medical bills.
3 tips for talking to your doctor
These principles can go a long way when communicating with your healthcare provider and establishing a relationship with them.
- Open communication: Be clear and upfront about your billing status and how you intend to pay your bills.
- Proactive approach: Ask upfront for itemized bills and about discounts that are available to you. Ask questions to aid your understanding of their billing process.
- Owning the “stewardship” responsibility that all Christians share: Be diligent to negotiate fair pricing with your providers and be quick to pay them fully for services they’ve rendered.
Healthcare providers: steps for successful interactions
We’ve worked with more than 100,000 healthcare providers nationwide, and we’re sharing our best tips from personal experience and from what CHM members have shared with us.
Tell your provider that you’re eager to pay your bills: Build rapport with your provider; when they know you want to pay your bills, the conversation will go more smoothly. Plus, it’s a testimony to others when we, as Christians, are determined to “do right” by them.
Communicate your billing status: Tell your healthcare providers that you’re uninsured and should be billed as a self-pay patient. We recommend telling your provider: “I don’t have insurance. I have something better: Christian Healthcare Ministries, which is a health cost sharing organization. Please apply any available uninsured or self-pay discounts to my bill.”
Your CHM card is not an insurance card. However, if your provider has a prearranged discount with CHM (see the “CHM friendly-providers” lookup tool on your Member Portal), show your card to your provider to identify yourself as a CHM member to take advantage of the discounts.
Self-pay versus uninsured:
- What is self-pay? It means you are paying your medical bills yourself rather than the provider billing insurance. A self-pay patient may or may not have traditional insurance. Most providers offer discounts for self-pay patients.
- “Uninsured” refers to people without health insurance. CHM isn’t insurance, and, if you don’t have a primary health insurance, you’re considered uninsured; however, CHM is an exemption to the Affordable Care Act and as such is an eligible option under the national healthcare law. Providers often offer discounts or options for people without insurance.
Ask for three things: 1) to be billed directly, 2) that bills are itemized, and 3) that any available self-pay or uninsured discounts are listed. As you submit bills to CHM, be sure to reference the CHM Guidelines for sharing eligibility. An itemized bill contains:
- Patient’s name
- Date of service
- Place of service
- Procedural (CPT) code or description of service
- Charge for each service
Avoid aggressive prepayment practices by calling CHM first: Please don’t pay upfront (unless the bill is less than $1,000).
A provider may require upfront payment or offer a discount only when services are paid upfront. However, the cost may have been marked up and still be over fair market value after the discount applies.
That’s why we recommend, prior to paying bills totaling $1,000 or more from an individual healthcare provider, contacting Member Advocate by calling 800-791-6225 when the following circumstances apply:
- You’re unable to obtain a self-pay discount
- You obtain a discount, but the provider requires payment upfront or has a deadline for payment.
If required to pay upfront for a surgery: Contact CHM’s Complete Surgical Care Solution (CSCS) team if you’ve been recommended surgery and have a diagnosis. CSCS matches you with a quality provider offering services at a fair-market price. You get the care you need and CHM takes care of the rest, by paying your provider directly for eligible bills. From January-April 2025, CHM members through CSCS saved $2.5 million in medical costs!
Ask about other financial assistance available: Apply for any financial assistance available to you, even if you don’t think you qualify.
As you ask, know that most hospitals are required to provide certain types of medical care at a reduced cost, so don’t be afraid to advocate for yourself. As self-pay, uninsured patients, CHM members may qualify for financial assistance programs which are offered by the hospital. Likewise, state and federal governments also allocate money toward healthcare for individuals whose incomes fall within a defined economic level.
Work together to create a strategy: Work with your provider to set up a monthly payment plan until your eligible medical costs have been processed and reimbursed in accordance with the CHM Guidelines.
Promptly pay your providers with your CHM sharing funds: Every membership unit must satisfy an annual Personal Responsibility; this is considered your out-of-pocket expense. Once this amount is met, you will receive reimbursement for the remaining eligible medical costs. It is your responsibility to use funds received from CHM to pay the appropriate healthcare providers.
Maternity only: If you have a maternity event, learn more about specific steps to take when communicating with your providers and how CHM can support you.
Communication in healthcare
As you follow these steps, you’ll be on your way to building an effective, professional relationship with your healthcare provider.
Being a self-pay, uninsured patient gives you the perks, flexibility, and opportunity to make the best decisions for your medical care. It’s another great advantage of being a part of the CHM family.
Being engaged in your healthcare decisions makes all the difference. The more you talk with your providers, the more you’ll be equipped to navigate the marketplace with ease. Plus, remember that the CHM staff is standing by, ready and willing to help along the way!
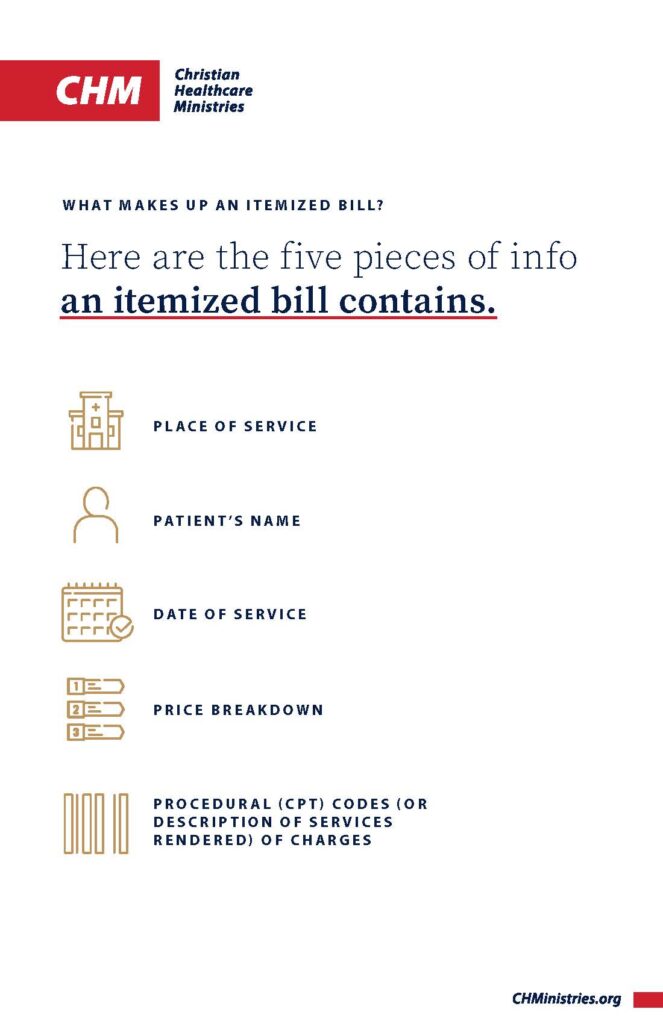
What is an itemized bill?
Save this pocket-sized explanation of the five elements that are included on an itemized bill. Bringing this handy tool will enable you to explain what you need so CHM can process your sharing request.




